The Glymphatic Pathway: Evaluating Neurological Conditions From a New Perspective
This complex waste clearance pathway within the CNS plays a crucial role in maintaining brain homeostasis, as a mechanism of protein waste removal alongside autophagy and protein aggregate ubiquitination.

Kevin Chang, PharmD

THE GLYMPHATIC SYSTEM is a complex waste clearance pathway within the central nervous system that plays a crucial role in maintaining brain homeostasis, particularly because—unlike other tissues in the body—the brain lacks a traditional lymphatic system.1 Prior to the discovery of the glymphatic system in 2012,2 it was thought that only the blood-brain barrier tightly regulated the exchange of macromolecules between the bloodstream and the brain3 and that the primary mechanism for removal of protein waste was autophagy and ubiquitination of protein aggregates.2-4
The glymphatic system relies on the continuous interchange of cerebrospinal fluid (CSF) and interstitial fluid (ISF)—facilitated by aquaporin 4 (AQP4) water channels (FIGURE2,4-6)—through the brain’s extracellular space to clear metabolic waste products and maintain a healthy environment for neuronal function.1 The glymphatic system operates via a process involving convective bulk flow, with CSF entering the brain’s extracellular space and mixing with ISF.1 This exchange is crucial for clearing metabolic waste found in the brain. The bulk flow is thought to be driven by arterial pulsation, which creates pressure gradients that propel the movement of CSF.3,7 The pulsation of arteries contributes to the directional flow of CSF from Virchow-Robin spaces (perivascular spaces surrounding small vessels) into the brain parenchyma, facilitating waste clearance.7
Sleep and wakefulness are also tied to glymphatic function. During sleep, the glymphatic system becomes 90% more active than during the wake state.8 As demonstrated in murine models, natural sleep or anesthesia is associated with a 60% increase in ISF volume,8 and this expansion promotes more efficient clearance of neurotoxic waste metabolites.4 On the other hand, sleep deficiency reduces perivascular flow9,10 and may lead to structural changes in perivascular spaces, which could explain the association between sleep disturbances and various neurological disorders such as Alzheimer disease (AD) and Parkinson disease.7
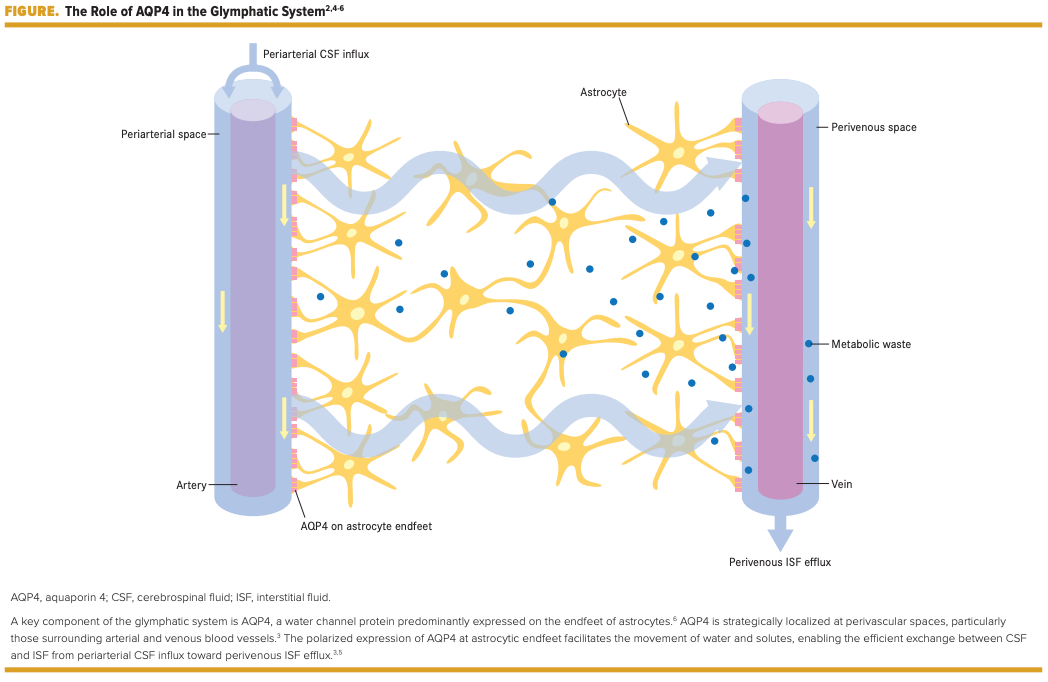
AQP4 mislocalization has been linked to glymphatic failure, increasing the risk of neurological dysfunction.7 When AQP4 is not properly polarized at astrocytic endfeet, the ability to clear waste metabolites is diminished, which may contribute to the aggregation of amyloid-β (Aβ) and tau, proteins associated with neurodegeneration.11 AQP4 and Aβ clearance have also been studied in the preclinical context of AQP4 knockout mice. In one study, researchers found that AQP4 knockout mice showed a 55% reduction in glymphatic clearance of radiolabeled Aβ compared with wild-type mice.2 In AD, the loss of AQP4 polarization is correlated with “increasing Aβ plaque density and worsening [AD] status,”7 highlighting the significance of AQP4 in maintaining glymphatic function. Loss of AQP4 polarity at astrocytic endfeet has also been correlated with Aβ burden and is a predictor of AD status.12 Arighi and colleagues found a “significant difference in AQP4 levels [in CSF between patients with AD] and the control group (AD 350.4 ±32.7 pg/ml vs controls 209.6 ±23.4 pg/ml).”1 The results from this study suggest that glymphatic dysfunction—as measured by increased AQP4 in CSF—and neurodegeneration have a synergistic feed-forward relationship.1,4
With the current understanding of the glymphatic system, researchers can explore novel therapeutic targets and methodologies. Because arterial pulsation is thought to be the primary driver of bulk flow, dobutamine may be another potential intervention; mice injected with this inotropic adrenergic agonist exhibited an acute increase in CSF-ISF exchange.2 Besides waste clearance in the central nervous system, the glymphatic system also functions to distribute necessary nutrients and solutes to the brain through CSF-ISF exchange.7 Utilizing this exchange presents a unique method to bypass the blood-brain barrier for delivery of therapeutic treatments such as adeno-associated viruses via intracranial injection13 and antisense oligonucleotides via lumbar intrathecal injection.14 The relationship between sleep and the glymphatic system also raises the possibility of evaluating therapeutic options that can sustain slowwave sleep or anesthetics to increase glymphatic clearance.7,15 In the context of dementia, glymphatic failure preceded Aβ deposition in murine models16 and, more recently, diminished Aβ clearance was shown to predict the disease burden of dementia and could be a potential early biomarker.17
The glymphatic pathway presents a new perspective from which to evaluate the brain’s relationship to sleep, CSF-ISF flow, and various neurological conditions. The intricate functioning of the glymphatic system not only underscores its pivotal role in waste clearance and brain homeostasis but also provides a critical lens through which its potential implications for neurological diseases may be examined. Understanding the interplay between the glymphatic system and neurological diseases enhances our comprehension of these complex conditions and opens avenues for exploring therapeutic interventions that target the glymphatic pathway to potentially mitigate the impact of neurodegeneration.
For correspondence:
Kevin Chang, PharmD
kevinchang1@gmail.com
REFERENCES
1. Sun C, Shen L, Zhang Z, Xie X. Therapeutic strategies for Duchenne muscular dystrophy: an update. Genes (Basel). 2020;11(8):837. doi:10.3390/genes11080837
2.De Stefano MA, Ambrosio R, Porcelli T, Orlandino G, Salvatore D, Luongo C. Thyroid hormone action in muscle atrophy. Metabolites. 2021;11(11):730. doi:10.3390/metabo11110730
3.Bloise FF, Oliveira TS, Cordeiro A, Ortiga-Carvalho TM. Thyroid hormones play role in sarcopenia and myopathies. Front Physiol. 2018;9:560. doi:10.3389/fphys.2018.00560
4. Gloss D, Moxley RT 3rd, Ashwal S, Oskoui M. Practice guideline update summary: corticosteroid treatment of Duchenne muscular dystrophy: report of the Guideline Development Subcommittee of the American Academy of Neurology. Neurology. 2016;86(5):465-472. doi:10.1212/WNL.0000000000002337
5. Davies TF, Latif R. Targeting the thyroid-stimulating hormone receptor with small molecule ligands and antibodies. Expert Opin Ther Targets. 2015;19(6):835-847. doi:10.1517/14728222.2015.1018181
6. Tedeschi L, Vassalle C, Iervasi G, Sabatino L. Main factors involved in thyroid hormone Action. Molecules. 2021;26(23):7337. doi:10.3390/molecules26237337
7. Ambrosio R, De Stefano MA, Di Girolamo D, Salvatore D. Thyroid hormone signaling and deiodinase actions in muscle stem/progenitor cells. Mol Cell Endocrinol. 2017;459:79-83. doi:10.1016/j.mce.2017.06.014
8. Salvatore D, Simonides WS, Dentice M, Zavacki AM, Larsen PR. Thyroid hormones and skeletal muscle--new insights and potential implications. Nat Rev Endocrinol. 2014;10(4):206-214. doi:10.1038/nrendo.2013.238
9. Bloise FF, Cordeiro A, Ortiga-Carvalho TM. Role of thyroid hormone in skeletal muscle physiology. J Endocrinol. 2018;236(1):R57-R68. doi:10.1530/JOE-16-0611
10. Taglietti V, Kefi K, Rivera L, et al. Thyroid-stimulating hormone receptor signaling restores skeletal muscle stem cell regeneration in rats with muscular dystrophy. Sci Transl Med. 2023;15(685):eadd5275. doi:10.1126/scitranslmed.add5275