
Duchenne Muscular Dystrophy progresses with motor delays, varying deterioration rates, and impacts multiple organs, highlighting the need for early intervention.
Pediatric neurologist, Children’s Health; assistant professor, UT Southwestern Medical Center; center director, Cure SMA Care Center; and co-director, Muscular Dystrophy Association Clinic–Dallas

Duchenne Muscular Dystrophy progresses with motor delays, varying deterioration rates, and impacts multiple organs, highlighting the need for early intervention.

Explore the comprehensive comorbidities of Duchenne Muscular Dystrophy, including cognitive, respiratory, and nutritional challenges faced by patients.

Duchenne Muscular Dystrophy progresses with motor delays, varying deterioration rates, and impacts multiple organs, highlighting the need for early intervention.

An expert discusses strategies to lower the age of Duchenne muscular dystrophy (DMD) diagnosis, emphasizing the importance of universal newborn screening with the testing of creatine kinase (CK) levels, clinician recognition of motor red flags such as the Gower sign, early neurology referrals, and incorporating CK level testing in cognitive delay evaluations to enable timely therapeutic intervention and improve long-term outcomes.

An expert discusses the typical presentation and diagnosis of Duchenne muscular dystrophy (DMD) around ages 5 to 6, highlighting early signs such as motor delays, Gower sign, and developmental concerns, while emphasizing the importance of newborn screening, clinician awareness, and developmental monitoring to enable earlier intervention and improved outcomes.

An expert discusses the critical role of dystrophin in maintaining muscle integrity across multiple systems, explaining how its absence in Duchenne and Becker muscular dystrophy leads to widespread complications—including neurologic, pulmonary, cardiac, gastrointestinal, urinary, and orthopedic issues—driven by chronic muscle damage, inflammation, and fibrosis.

An expert discusses the evolving treatment landscape of Duchenne muscular dystrophy (DMD), highlighting advances in gene therapy, exon-skipping agents, and novel corticosteroids that aim to slow disease progression, improve muscle function, and enhance quality of life, while emphasizing the growing role of personalized medicine and early intervention in optimizing long-term outcomes.
The neuromuscular specialist at the Neurology & Neuromuscular Care Center discussed the pressing need to address the transition of care from pediatric to adult healthcare systems in Duchenne muscular dystrophy. [WATCH TIME: 6 minutes]
Closing thoughts on advice to community neurologists treating spinal muscular atrophy (SMA).

Experts remind families of the importance of follow-up visits with the multidisciplinary team during COVID-19.
Resources are discussed, including the Child Neurology Foundation’s telehealth tip sheet, to help families navigate telehealth.
Several spinal muscular atrophy (SMA) resources are suggested to help physicians and families, including Cure SMA and standard of care guidelines.
Discussing the diagnosis of spinal muscular atrophy (SMA) with the family and lining up appointments with the multidisciplinary team to help care for the patient.
Diana Castro, M.D., stresses the value of the initial in-person neurology visit for evaluation of spinal muscular atrophy (SMA) to ensure a correct diagnosis. The next step in the process would be genetic testing.
The signs and symptoms leading a pediatrician to a diagnosis of spinal muscular atrophy (SMA) are discussed.
Diana Castro, M.D., discusses newborn screening for spinal muscular atrophy (SMA) and suggests how to care for patients after the results are received.
Early recognition and referral of a patient with suspected spinal muscular atrophy (SMA) to a neurologist.
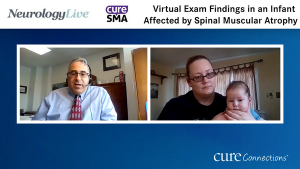
Garey H. Noritz, MD, walks us through a virtual pediatric neurological exam and notes examination findings that may be identified in an infant with Spinal Muscular Atrophy (SMA).
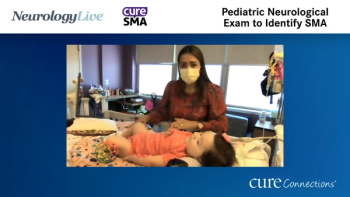
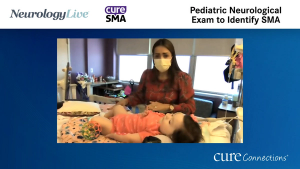
Diana Castro, MD walks us through a pediatric neurological exam and notes examination findings that may be identified in an infant with Spinal Muscular Atrophy (SMA).
Published: March 22nd 2021 | Updated:
Published: March 22nd 2021 | Updated:
Published: March 11th 2021 | Updated:
Published: March 11th 2021 | Updated:

Published: March 22nd 2021 | Updated:
Published: March 18th 2021 | Updated: