Blog
Article
If the First Migraine Treatment Fails, Try, Try Again
Author(s):
Some migraine sufferers who do not initially respond to galcanezumab may show clinically meaningful improvement if they stay on the drug for longer periods of time.

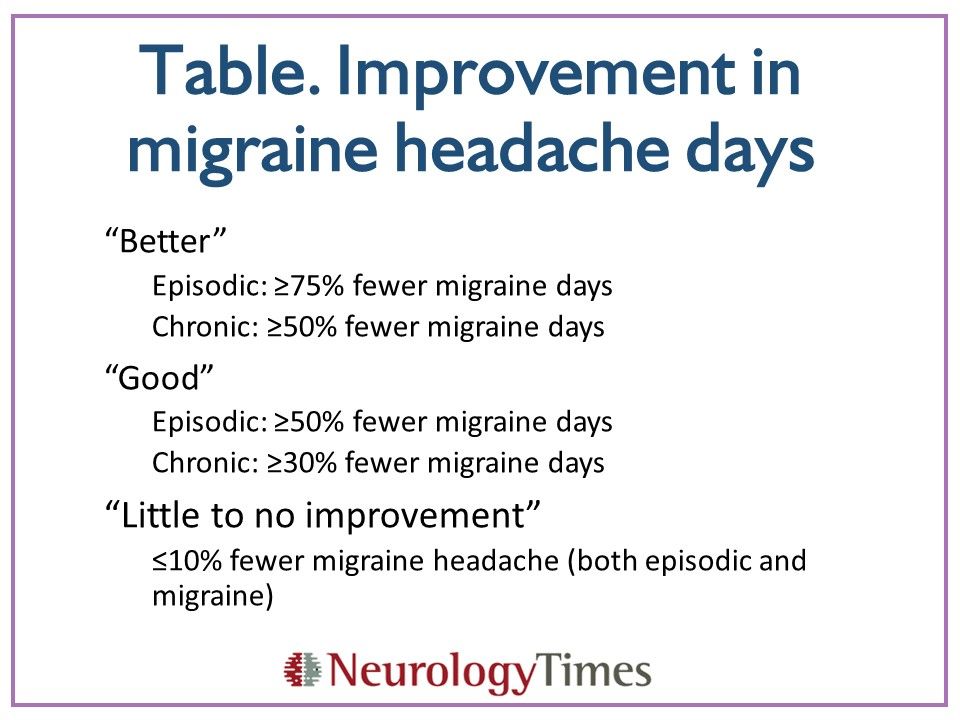
Table
RESEARCH UPDATE
Some migraine sufferers who do not initially respond to galcanezumab may show clinically meaningful improvement if they stay on the drug for longer periods of time, according to a study by Nichols and colleagues.1
“Galcanezumab-treated patients with episodic or chronic migraine who have not responded following 1 or 2 months of treatment appear to have a reasonable likelihood of continued improvement in months following initial treatment, with greater likelihood seen in patients showing greater early improvement,” wrote first author Russell Nichols, PharmD, of Eli Lilly and Company, Indianapolis, IN. “Factors contributing to response/nonresponse have yet to be elucidated and clinical judgment should be exercised when deciding whether to discontinue treatment,” they added.
Galcanezumab is a monoclonal antibody that blocks calcitonin gene-related peptide (CGRP) receptors involved in migraine development. The drug was approved in September 2018 for migraine prevention in adults.2
The FDA approval was largely based on results from three randomized, double-blind placebo-controlled studies.3-5 The first two, EVOLVE-13 and EVOLVE-2,4 included over 1700 participants with episodic migraine who were randomized for six months of subcutaneous injections of galcanezumab 120 mg/month or 240 mg/month, or placebo. Results showed that about 60% of participants achieved a clinically meaningful reduction in monthly migraine days (≥50% reduction from baseline).
The third trial was called REGAIN and included over 1100 participants with chronic migraine randomized to the same doses of galcanezumab or placebo for three months.5 Results showed that over one quarter of the galcanezumab groups reached clinically meaningful reductions in monthly migraine days.
Results also suggested that patients who did not respond in the first month showed improved responses with continued use. To investigate the issue, researchers conducted a post-hoc analysis of these nonresponders.
The analysis included 879 EVOLVE-1 and EVOLVE-2 participants with episodic migraine and without good early improvement (≥ 50% reduction in monthly migraine days). It also included 555 REGAIN participants with chronic migraine without good early improvement (≥30% reduction monthly migraine days). Participants included in the analysis were over 80% female, over 74% white, and had a mean age of 40 years.
Researchers further divided participants according to level of reduction in migraine headache days (modest, limited, minimal/no improvement or worsening) over one month and over one or two months.
Finally, they pooled data for the galcanezumab groups and calculated percentages of patients categorized according to improvement in migraine headache days with continued treatment (Table).
Results for episodic migraine showed that more patients with modest response at one month achieved “good” (62%) or “better” (20%) responses with continued treatment, compared to participants with less robust responses at one month. Forty-three percent of those with initial limited response achieved “good” response, while 34% of those with initial minimal/no early improvement achieved “good” responses. Twenty percent of those with initial worsening symptoms showed a good response with continued treatment. Still, about 10% of these patients experienced “better” response with continued treatment.
Results were similar for chronic migraine. Of those with modest early improvement at one month, 38% achieved “good” and 13% achieved “better” responses with continued treatment. About 17% of those with minimal/no early improvement and 11% with worsening symptoms achieved “good” response with continued treatment. Only about 4% with minimal/no improvement or worsening symptoms achieved a better response.
Results showed a similar pattern among participants with initial nonresponse at one or two months, though with lower percentages.
The authors noted that the best predictor of “good” response with continued treatment was whether an individual achieved modest improvement within the first month of taking galcanezumab.
They also noted several limitations. All three trials were of relatively short duration, and effects of treatment with galcanezumab beyond six months are unknown. For chronic migraine, the analysis defined “good” response as ≥30% reduction in migraine days, while a clinically meaningful difference is often considered to be ≥50% reduction. However, given the challenges of treating chronic migraine ≥30% reduction may be clinically relevant, according to the authors.
Take Home Points
• Post-hoc analysis of participants in EVOLVE-1, EVOLVE-2 and REGAIN who did not respond in the first one or two months of receiving galcanezumab showed those with modest early response are more likely to achieve “good” response with continued treatment than those with less robust initial response.
• 62% with episodic headache and modest response at one month showed achieved “good” response with continued treatment
• 20% with chronic headache and modest response at one month showed achieved “good” response with continued treatment
• Results were similar but with lower percentages for chronic migraine, and for noresponders within the first one or two months of initial treatment
References:
1. Nichols R, Doty E, Sacco S, et al. Analysis of Initial Nonresponders to Galcanezumab in Patients With Episodic or Chronic Migraine: Results From the EVOLVE-1, EVOLVE-2, and REGAIN Randomized, Double-Blind, Placebo-Controlled Studies. Headache. 2018; Nov 21 [Epub ahead of print].
2. Ely Lilly. Lilly's Emgality™ (galcanezumab-gnlm) Receives U.S. FDA Approval for the Preventive Treatment of Migraine in Adults. https://investor.lilly.com/news-releases/news-release-details/lillys-emgalitytm-galcanezumab-gnlm-receives-us-fda-approval. Accessed January 1, 2019.
3. Stauffer VL, Dodick DW, Zhang Q, et al. Evaluation of Galcanezumab for the Prevention of Episodic Migraine: The EVOLVE-1 Randomized Clinical Trial. JAMA Neurol. 2018;75:1080-1088.
4. Skljarevski V, Matharu M, Millen BA, et al. Efficacy and safety of galcanezumab for the prevention of episodic migraine: Results of the EVOLVE-2 Phase 3 randomized controlled clinical trial. Cephalalgia. 2018;38:1442-1454.
5. Detke HC, Goadsby PJ, Wang S, et al. Galcanezumab in chronic migraine: The randomized, double-blind, placebo-controlled REGAIN study. Neurology. 2018;91:e2211-e2221.
Newsletter
Keep your finger on the pulse of neurology—subscribe to NeurologyLive for expert interviews, new data, and breakthrough treatment updates.