“ACCESS TO AFFORDABLE, appropriate, high-quality health care is essential for people with MS [multiple sclerosis] to live their best lives,” according to the National MS Society.1 Generics and biosimilars have the potential to contribute to the realization of this principle.
Although there are known obstacles that play a role in the use of generics and biosimilars in the United States, generics and biosimilars are important treatment options because they have no clinically meaningful differences from their reference medicines. In looking at other disease states or other countries where generics and biosimilars are encompassed within the standard of care, we see that the emergence and growth of generic and biosimilar disease-modifying therapies (DMTs) can increase market competition, increase access, and drive costs down for patients over time, leading to improved adherence, helping to contain health care costs, and leading to a reduction in health disparities and a more equitable health care system.2
Landscape
The Beginning of the Biosimilars Era in Multiple Sclerosis
Jeff Cohen, MD; Alycin Magruder, PharmD; and Sarah Anderson, PharmD, discuss the downstream effects for physicians, patients, and payers in this new era of treatment in MS.
View video:
neurologylive.com/biosim-roundtable
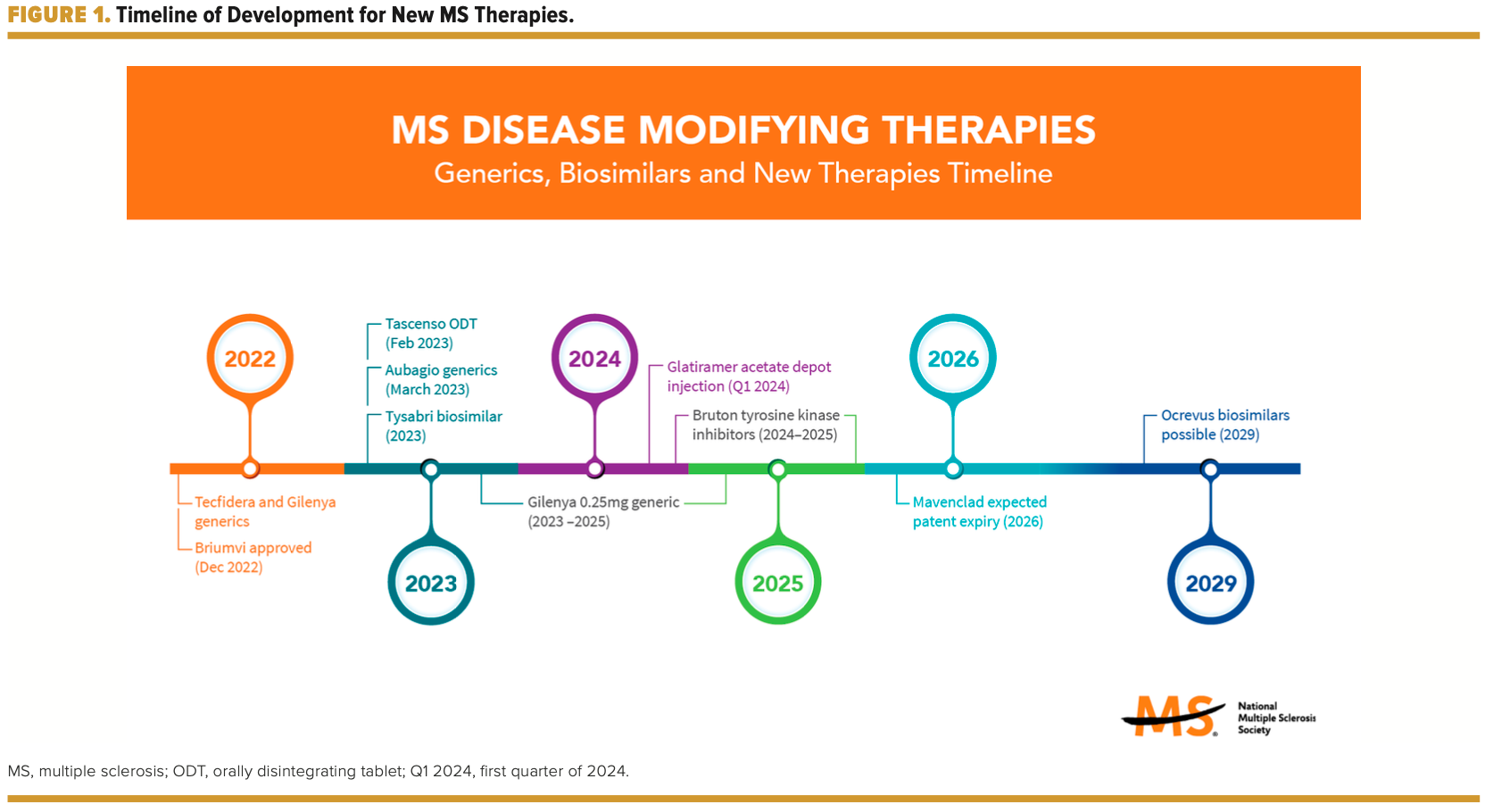
The landscape of DMTs has evolved from 0 treatments available prior to 1993 to more than 20 medications available in 2023 (FIGURE 1). In addition to DMT generics and now the FDA approval of the first DMT biosimilar, a natalizumab biosimilar, the DMT pipeline holds the potential for additional biosimilars being developed as well as a new class of medications seeking FDA approval. Options have increased for patients with MS and their health care providers to cocreate treatment regimens and participate in shared decision-making. Often, insurance coverage, cost, availability of financial assistance, and access drive treatment decisions. The availability of generics and biosimilars in the MS space is a step in the right direction to increase access and improve affordability of medications.
Accessibility and Affordability
The annualized list price of DMTs ranges from $2700 to more than $127,000. MS is a financially burdensome disease, and pharmacotherapy contributes to a significant portion of its costs. Specialty medications used to manage autoimmune conditions represent $1 of every $5 in drug expenditures.3
Although the wholesale cost of generics and biosimilars is less than the originator products, the cost to the patient may be more than what they pay for the originator product because of insurance coverage and the financial assistance they received from the manufacturer of the reference medicine. Often, once generics hit the market, the financial assistance offered by the manufacturer of the reference medicine is eliminated. Generic manufacturers may offer drug coupon cards, but there may be certain eligibility criteria associated with their use. Health plans and health systems need to make decisions about whether and where to place generics and biosimilars on the formulary, which would affect the cost responsibility of the patient. Infusion centers need to make decisions about which biosimilar to supply when there are multiple biosimilars available for a given biologic. All these decisions affect medication accessibility and affordability for patients.
Improving the accessibility and affordability of these medications will take both time and multistakeholder collaboration. An area where providers can make an impact is education. Patients need to understand how these medications are approved by the FDA, receive assurance by their provider that these medications are not only deemed acceptable but safe and effective as their reference medicines, have access to them, and be able to afford them. The remainder of this article will focus on how providers can engage patients on the topics of approvability and acceptability.
Approvability
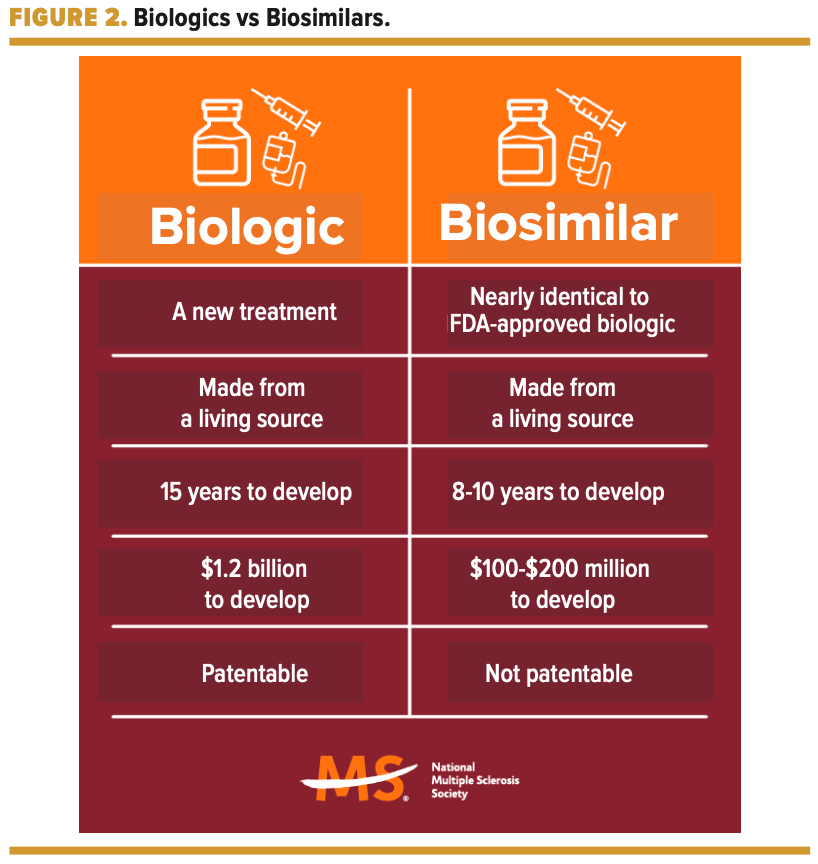
Generic and biosimilar manufacturers must show that there are no clinically meaningful differences in the safety, efficacy, and potency of follow-on medications when compared with the reference medicine. Although generics are chemically synthesized and are a copy of the branded product, biosimilars are not an exact copy of the original biologic. Biosimilars have the same amino acid sequence, route of administration, and strength as their reference biologic. However, because biologics and biosimilars are made from living sources, they display a certain degree of variability, even within or between different batches of the same medicine in the form of different glycosylation patterns.4 Slight variations are expected and clinically acceptable because the FDA requires that these variations are carefully controlled, monitored, and kept within acceptable limits. Biosimilarity of the biosimilar to the reference biologic is showcased by demonstrating the equivalence of structural, functional, and pharmacokinetic/pharmacodynamic profiles and through clinical confirmation of similarity in efficacy, safety, and immunogenicity in a specific population.5
Acceptability
The nocebo effect is a phenomenon that can have an impact on patient perceptions of follow-on medications. There are concerns among some providers that cheaper follow-on DMTs are only produced to reduce costs to the health care system and that the well-being and safety of patients are not prioritized when manufacturing and approving such medications.6 Gaps in knowledge about how follow-on medications are approved contribute to safety and efficacy concerns, avoidance of prescribing follow-on DMTs, nocebo effects, and nonadherence.7 Follow-on medications take less time to develop and cost less to develop in part because the discovery phase is not needed and there are typically fewer marketing and advertising costs (FIGURE 2). To learn more about how follow-on medications are approved, reference the FDA website.
If the provider and patient have negative expectations of generics and biosimilars going into a treatment switch, the treatment can result in poorer outcomes.8 Patients look to providers when developing their perceptions, expectations, and judgments regarding any given treatment. By taking the time to address fears, concerns, and challenges that patients voice regarding their treatment options, providers can play a key role in the adoption of generics and biosimilars in the MS space. Arming patients with assistance to support financial needs is another critical component. To ensure patients have fully explored all cost considerations, it may be valuable to identify whether they are aware
they have access to tools and resources to help them understand
stand the following:
- Their health plan’s formulary design
- Applicable pharmacy and/or medical benefits related to DMT coverage
- Potential eligibility for the manufacturer’s patient assistance programs
- Access to a specialty pharmacist for support services
- Options to access a given medication
- Options for where they can receive the lowest price for their medication
If patients are not aware of tools and resources available, referring them to appropriate staff, such as the National MS Society’s MS Navigator program, may be warranted. Ultimately, providing reputable resources to reduce patient confusion and fostering an environment of shared decision-making with patients will result in high patient satisfaction, improved outcomes, and decreased costs to patients and the health care system.
Additional Research and Pharmacovigilance Are Warranted
Key Takeaways
Enhancing Access to MS Treatment: Recognize the role of generics and biosimilars in providing affordable and high-quality care for individuals with multiple sclerosis (MS), ultimately contributing to improved adherence, cost containment, and a more equitable healthcare system.
Navigating Accessibility Challenges: Acknowledge the evolving landscape of disease-modifying therapies (DMTs) for MS, the financial burden faced by patients, and the potential impact of generics and biosimilars on increasing accessibility. Understand the complexities in decisions made by health plans, health systems, and infusion centers that influence medication accessibility and affordability.
Provider Role in Patient Education: Understand the significance of education in addressing patient concerns about the approvability and acceptability of generics and biosimilars. Emphasize the FDA's rigorous approval process, ensuring patients are informed about the safety, efficacy, and equivalence of follow-on medications. Providers play a crucial role in dispelling misconceptions, addressing fears, and supporting shared decision-making, ultimately optimizing individualized treatment and fostering a collaborative healthcare approach.
Rituxan and rituximab biosimilars have been used off label to manage MS for some time. Findings from studies of Rituxan and the rituximab biosimilars in MS have shown that the biosimilars have similar efficacy, safety, and tolerability as the reference product.9 The clinical relevance of antidrug antibodies remains unknown, and further studies are needed to obtain data on antidrug antibodies between the biosimilar(s) and originator.10 Because immunogenicity is a concern with the biologics and biosimilars used to manage MS, particularly when considering multiple switching or cross-switching, it will be imperative to better understand and either validate or invalidate these concerns through clinical studies. In addition, advocating for further research and patient registries to better track long-term pharmacovigilance data is critical. Being transparent with patients about this and encouraging open lines of communication to track what they are taking, the manufacturer of their medication, and what their experience with a given medication looks like are important.
Conclusions
There are multiple stakeholders who are responsible for clear communication, sharing reputable unbiased education via multiple modalities, combating misinformation, and supporting long-term pharmacovigilance efforts. With a collaborative care team approach, providers can offer treatment options and leverage pharmacists to aid in treatment decisions, patient education, addressing patient concerns, and ensuring accessibility and affordability. Empowering patients in shared decision-making with the support of the care team can optimize individualized treatment and benefit the health care ecosystem. Providing relevant and accurate information about generics and biosimilars has the potential to increase appropriate use of these medications and positively affect equity within the health care ecosystem.
REFERENCES
1. Access to high quality MS healthcare principles. National MS Society. 2021. Accessed September 15, 2023. https://www.nationalmssociety.org/Get-Involved/Advocate-for-Change/Take-Action/Access-to-High-Quality-Healthcare/Access-to-High-Quality-MS-Healthcare-Principles
2. Boccia R, Jacobs I, Popovian R, de Lima Lopes G Jr. Can biosimilars help achieve the goals of US health care reform? Cancer Manag Res. 2017;9:197-205. doi:10.2147/CMAR.S133442
3. Bowen K, Starner CI, Gleason PP. Prevalence and cost of autoimmune specialty drug use by indication in a commercially insured population, January 2019 through June 2020. Prime Therapeutics. April 2021. Accessed October 1, 2023. https://www.primetherapeutics.com/wp-content/uploads/2021/09/SP_AMCP_-S21_AutoImmune.pdf
4. Biosimilars info sheetlevel 2: regulatory and scientific concepts. FDA. Accessed September 15, 2023. https://www.fda.gov/media/154915/download
5. Markus R, Liu J, Ramchandani M,Landa D, Born T, Kaur P.Developing the totality of evidence for biosimilars: regulatory considerations and building confidence for the healthcare community. BioDrugs. 2017;31(3):175-187. doi:10.1007/s40259-017-0218-5
6. Rivera VM. Biosimilar drugs for multiple sclerosis:an unmet international need or a regulatory risk? Neurol Ther. 2019;8(2):177-184.doi:10.1007/s40120-019-0145-0
7. Greene L, Singh RM, Carden MJ, Pardo CO, Lichtenstein GR. Strategies for overcoming barriers to adopting biosimilars and achieving goals of the Biologics Price Competition and Innovation Act: a survey of managed care and specialty pharmacy professionals. J Manag Care Spec Pharm.2019;25(8):904-912. doi:10.18553/jmcp.2019.18412
8. Kristensen LE, Alten R, Puig L, et al. Non-pharmacologicaleffects in switching medication: the nocebo effect in switching from originator to biosimilar agent. BioDrugs. 2018;32(5):397-404. doi:10.1007/s40259-018-0306-1
9. Perez T, Rico A,Boutière C, et al. Comparison of rituximab originator (MabThera) to biosimilar (Truxima) in patients with multiple sclerosis. Mult Scler. 2021;27(4):585-592. doi:10.1177/1352458520912170
10. Dunn N, Juto A, Ryner M, et al. Rituximab in multiple sclerosis: frequency and clinical relevance of anti-drug antibodies. Mult Scler. 2018;24(9):1224-1233. doi:10.1177/1352458517720044