In a recent study utilizing data from 2 longitudinal cohorts, results showed that the lysosomal pathway is associated with an earlier progression of cognitive decline in patients with Parkinson disease (PD) who have a low risk for Alzheimer disease (AD). These results support the complex interplay between genetics and neuropathology in PD-related cognitive impairment, highlighting the role of lysosomal polygenic burden.1
In this analysis, investigators assessed data from 374 patients with PD from the Parkinson's Progression Markers Initiative (PPMI) cohort and 777 patients with PD from the Parkinson's Disease Biomarker Program (PDBM) cohort. Among both datasets, authors observed an association between lysosomal polygenic score and faster progression of cognitive decline in those with low AD risk (P = 0.0032 and P = 0.0054, respectively).
Top Clinical Takeaways
- The study emphasizes the significance of lysosomal genetics in cognitive decline progression in Parkinson disease, particularly in patients with low Alzheimer disease risk.
- Lysosomal polygenic scores were associated with faster cognitive decline in Parkinson with low Alzheimer risk, indicating a potential biomarker for prognosis.
- Further research with larger cohorts is necessary to validate these findings and explore their implications for precision medicine and therapeutic targets in Parkinson disease.
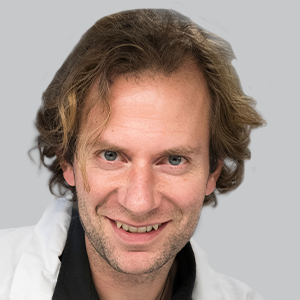
“We highlight the burden of lysosomal variants for cognitive progression in PD patients with a low vulnerability to AD copathology,” senior author Lasse Pihlstrøm, PhD, senior researcher in department of neurology at Oslo University Hospital in Norway, and colleagues, wrote.1 “Further, our results provide novel evidence for stratification by the polygenic burden of AD risk alleles, which may enable a more precise understanding of the genetic influence of cognitive decline in PD.”
READ MORE: Exposure to Trichloroethylene Linked With Increased Risk of Parkinson Disease, Cancer
Newly published in Movement Disorders, investigators used Cox regression to assess the association between lysosomal polygenic scores and time to Montreal Cognitive Assessment (MoCA)2 scores of less than 21 in the PPMI cohort, with replication of the data coming from the PDBP cohort. Authors noted that the PPMI data included cerebrospinal fluid (CSF) biomarkers of AD pathology at baseline. The study used data from 217 neuropathologically characterized Lewy body disease samples from the Netherland's Brain Bank to set an optimal threshold for AD polygenic risk score (PRS) to distinguish between samples with and without significant AD copathology.
In all participants from PPMI, the lysosomal PD-PRS did not show any significant association with time to dementia. In a subset of PPMI patients with negative AD CSF biomarkers, the lysosomal PD-PRS was associated with a faster cognitive decline (P = 0.039). Among AD CSF biomarkers, authors observed that the strongest association with cognitive decline in PD was with low CSF amyloid-β1-42 levels.
In a split of the PPMI samples based on AD-PRS, patients with a high vulnerability to AD copathology (n = 126) showed a significantly lower mean baseline CSF Aβ1-42 (P = 0.0025). Notably, in samples with a low vulnerability to AD copathology (n = 248), investigators observed a significant association between the lysosomal PD-PRS and a shorter time to dementia. When authors repeated this analysis excluding GBA1, the lysosomal PD-PRS remained significantly associated with a shorter time to dementia in PPMI participants who had a normal baseline CSF Aβ1-42 (HR, 1.45; 95% CI, 1.0–2.1; P = 0.0475) and in the PDBP patients with a low vulnerability to AD copathology (HR, 1.33; 95% CI, 1.05–1.67; P = 0.0162).
“Additionally, our results suggest lysosomal variants beyond GBA1 contribute to cognitive decline, as the association between the lysosomal PD-PRS excluding GBA1 and time to dementia remained significant in PPMI and PDBP [participants] with a low CSF and genetic vulnerability to AD copathology, respectively,” Pihlstrøm et al noted.1 “The present study [supports] that the cumulative lysosomal genetic burden is part of an overlapping genetic architecture of vulnerability to both more widespread Lewy pathology and earlier cognitive progression in PD.”
Authors acknowledged the study's limitations, including the sample size event, though the findings were replicated across both used cohorts. In addition, investigators noted that the study was not well-powered to explore the several different algorithm parameters for the PRS calculation such as P-value and clumping thresholds, which Pihlstrøm and colleagues noted should be optimized empirically in larger datasets ideally.
“Additional research with larger cohorts and more comprehensive assessment of cognition is needed to validate and expand on these findings. With further improvement, we hope that the PRSs may inform individual prognosis and facilitate detection of therapeutic targets within a precision medicine framework,” Pihlstrøm et al noted.1
REFERENCES
1. Tunold JA, Tan MMX, Toft M, Ross O, van de Berg WDJ, Pihlstrøm L. Lysosomal Polygenic Burden Drives Cognitive Decline in Parkinson's Disease with Low Alzheimer Risk. Mov Disord. 2024;39(3):596-601. doi:10.1002/mds.29698
2. Nasreddine ZS, Phillips NA, Bédirian V, et al. The Montreal Cognitive Assessment, MoCA: a brief screening tool for mild cognitive impairment [published correction appears in J Am Geriatr Soc. 2019 Sep;67(9):1991]. J Am Geriatr Soc. 2005;53(4):695-699. doi:10.1111/j.1532-5415.2005.53221.x