Pagan shared insights from InfusON patient interviews on the challenges and benefits of initiating CSAI therapy and discussed how expert roundtable recommendations can guide neurologists in managing skin nodules associated with treatment.
Pagan shared insights from InfusON patient interviews on the challenges and benefits of initiating CSAI therapy and discussed how expert roundtable recommendations can guide neurologists in managing skin nodules associated with treatment.

Panelists discuss how chronic inflammatory demyelinating polyneuropathy (CIDP) can significantly impair quality of life for both patients and caregivers, emphasizing that early recognition and timely treatment are essential to prevent irreversible damage and improve long-term outcomes.

The division chief of child neurology at Dayton Children’s Hospital discussed findings from a study comparing patient satisfaction scores between telehealth and in-person visits in pediatric epilepsy care. [WATCH TIME: 4 minutes]

Panelists discuss how treatment changes in Parkinson disease are necessitated by disease progression, diminishing medication effectiveness, and emerging motor complications, examining a physician’s systematic approach to treatment adjustments and the range of available options for managing off fluctuations.

Panelists discuss how off fluctuations in Parkinson disease become increasingly prevalent as the disease progresses, significantly impacting patient quality of life through reduced mobility, independence, and overall well-being.

The chief scientific officer at Precision Biosciences provided clinical commentary on ARCUS gene editing platform and its potential application in Duchenne muscular dystrophy through a durable, AAV-delivered therapeutic strategy. [WATCH TIME: 4 minutes]

The division chief of neurology at Nemours Children’s Hospital spoke on the need for timely referrals to epilepsy centers for patients with drug-resistant epilepsy. [WATCH TIME: 5 minutes]
The chief of ophthalmology at the Doheny Eye Institute discussed decades of research uncovering how Alzheimer can impact visual function and how retinal imaging may advance diagnosis. [WATCH TIME: 13 minutes]

The neuroradiologist at Mayo Clinic discussed the clinical and conceptual differences between Alzheimer disease diagnostic frameworks and how clinicians should prepare for a shifting treatment landscape. [WATCH TIME: 4 minutes]
Pagan discusses the excitement surrounding new therapeutics in neurodegenerative diseases and how advances in protein clearance and inflammation reduction could lead to disease-modifying treatments for conditions like Parkinson disease.

Panelists discuss how medical professionals adjust treatment regimens and create individualized plans as Parkinson disease advances in their patients.

Panelists discuss how medical professionals determine the most appropriate treatment options for patients with advanced Parkinson disease and the challenges patients face as their disease progresses over time.
Fernando L. Pagan, MD, discussed how continuous subcutaneous apomorphine infusion impacts long-term motor fluctuations in Parkinson disease, highlighting InfusON extension study findings on uninterrupted "good ON" time and reduced "OFF" periods as evidence of its real-world efficacy.
Neurology News Network. for the week ending April 19, 2025. [WATCH TIME: 3 minutes]

The resident in the Department of Neurology at NYU Langone Health discussed the preliminary findings of a 9-month study on lecanemab recently presented at the 2025 AAN Annual Meeting. [WATCH TIME: 2 minutes]
The former FDA commissioner discussed the collaborative power of the neuromuscular community and the challenges of implementing emerging therapies in a rapidly evolving care landscape. [WATCH TIME: 4 minutes]

The executive vice president of research at the National MS Society talked about how the award continues to honor transformative multiple sclerosis research and inspire the next generation of investigators. [WATCH TIME: 5 minutes]
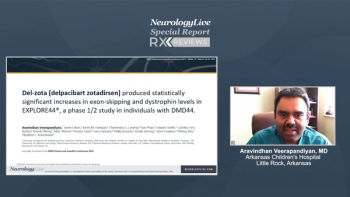
Aravindhan Veerapandiyan, MD, discusses how del-zota (delpacibart zotadirsen), an exon 44 skipping agent using antibody-conjugated phosphorodiamidate morpholino oligomer (PMO) technology, demonstrated favorable safety, significant dystrophin production (25% of normal), and unprecedented reduction of creatine kinase levels to near-normal in patients with Duchenne muscular dystrophy (DMD) during phase 1/2 clinical trials.

Panelists discuss how a careful, evidence-based approach combining clinical evaluation with electrodiagnostic and supportive findings is critical for accurately diagnosing chronic inflammatory demyelinating polyneuropathy (CIDP) and avoiding common misdiagnoses that can lead to inappropriate treatment.

Panelists discuss how recognizing the diverse clinical presentations and underlying immune mechanisms of chronic inflammatory demyelinating polyneuropathy (CIDP) is essential for accurate diagnosis, differentiating subtypes, and guiding effective, individualized treatment strategies.

Panelists discuss how cognitive testing tools, functional assessments, and biomarker integration guide Alzheimer disease diagnosis and staging, while early identification enables timely access to disease-modifying therapies, care coordination, and improved long-term outcomes.

Panelists discuss how early recognition of cognitive symptoms, timely referrals, multidisciplinary collaboration, and emerging diagnostic innovations are critical to diagnosing Mild Cognitive Impairment (MCI) and improving access to comprehensive Alzheimer disease care.
The chief scientific officer of the Parkinson’s Foundation discussed the foundation’s efforts to integrate whole genome sequencing into PD GENEration and expand access across diverse global populations. [WATCH TIME: 4 minutes]

A duo of neurology experts from Feinberg School of Medicine talked about the diagnostic challenges, evolving understanding, and clinical implications of paraneoplastic neurological syndromes. [WATCH TIME: 3 minutes]
The professor in the Department of Pathology and Laboratory Medicine at the University of California, Irvine, gave clinical insights on efforts to refine neuropsychological outcome measures for individuals with Down syndrome at risk for Alzheimer disease. [WATCH TIME: 3 minutes]

The chief scientific officer at Satellos Bioscience discussed phase 1 findings on SAT-3247, an oral AAK1 inhibitor, highlighting its safety, pharmacokinetics, and early translatability in Duchenne muscular dystrophy. [WATCH TIME: 7 minutes]
The director of NYU Langone's Multiple Sclerosis Comprehensive Care Center discussed the importance of early, high-efficacy treatment for pediatric MS. [WATCH TIME: 3 minutes]

The chief medical officer at Cognito Therapeutics provided a clinical overview on promising findings surrounding the company’s gamma sensory stimulation device in patients with Alzheimer disease. [WATCH TIME: 10 minutes]

The vice president of research at Cognition Therapeutics provided commentary on the safety of investigational CT1812 and its role in immune response and synapse-related pathways. [WATCH TIME: 3 minutes]

The senior director of mission programs at The ALS Association discussed how the thinkALS Toolkit can aid general neurologists in identifying and referring suspected cases more efficiently. [WATCH TIME: 5 minutes]