
Clinicians should use caution when prescribing this medication in patients with heart disease because of risk of severe adverse effects and even death. Test your skills in this FDA quiz.

Clinicians should use caution when prescribing this medication in patients with heart disease because of risk of severe adverse effects and even death. Test your skills in this FDA quiz.

In a head-to-head comparison, levetiracetam was shown to increase the rate of infants free of monotherapy failure by 28% more than phenobarbital in pediatric patients with nonsyndromic epilepsy.
In patients with epilepsy who live in western societies, suicide rates are increasing. Does culture play a role? Here's a study of Asian populations.

The smartwatch detected 40 generalized tonic-clonic seizures with 100% accuracy in a supporting clinical trial of 135 patients.

Although rare, new onset refractory status epilepticus can be life threatening if not identified quickly.

Starting eslicarbazepine acetate (ESL) at 400 mg daily may result in fewer adverse effects than starting at 800 mg for most patients with partial onset seizures.
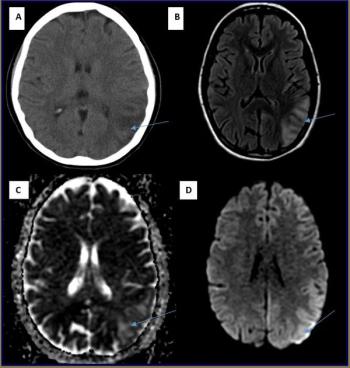
Differential diagnosis and treatment of mitochondrial encephalomyopathy lactic acidosis and stroke-like syndrome.
A summary of cutting-edge technology, including the world�’s smallest fully implantable spinal cord neurostimulator for the treatment of chronic pain.

The highest level of comprehensive care targets youths with epilepsy who have known comorbid psychiatric, developmental, and cognitive disorders and/or a history of nonadherence to seizure medication.
Which antiepileptic drugs work best as monotherapy? A new Cochrane meta-analysis scrutinizes the evidence.

Here's reason to start eslicarbazepine acetate at 400 mg daily.

A new study finds that children with epilepsy who are treated with antiepileptic drugs sustain more bone fractures than kids who don't take these drugs. Details here.

Most neurologists reach for levetiracetam monotherapy for children with early onset, nonsyndromic epilepsy initially. This study questions that practice.

Marijuana has been employed since ancient times for the treatment of epilepsy. However, rigorous scientific data supporting its efficacy has been essentially nonexistent until recently.
The authors present illustrative fictional accounts of patients with medical problems with co-occurring epilepsy.

Dietary therapies have returned to the spotlight as viable nonpharmacological treatment options for medication refractory epilepsy.

An update on responsive neurostimulation, the only implantable, closed-loop device approved for treating seizures.
3 things you may not know-from the new AAN guidelines-about sudden unexpected death in epilepsy.

Key details about an option for the treatment of drug-resistant epilepsy in patients who are not surgical candidates.
Dr. Loeb summarizes a global and one-of-a-kind approach of biomarker and drug discovery using systems biology of human brain tissues.

Thanks to technology, it may be possible to diagnose epilepsy in patients earlier and via noninvasive means.
Here: 3 questions that challenge your acumen about the latest AAN guidelines on sudden unexplained death in epilepsy.
What are the risks of anti-seizure meds in pregnancy? Benefits?
New studies shed light on topics such as nonencephalic pain and headache chronicity; benign childhood epilepsy with centrotemporal spikes and social cognition; and causal triggers of Alzheimer disease onset.

What do the new AAN guidelines on SUDEP offer? Here’s a quick overview of the key facts.